Wellness Center
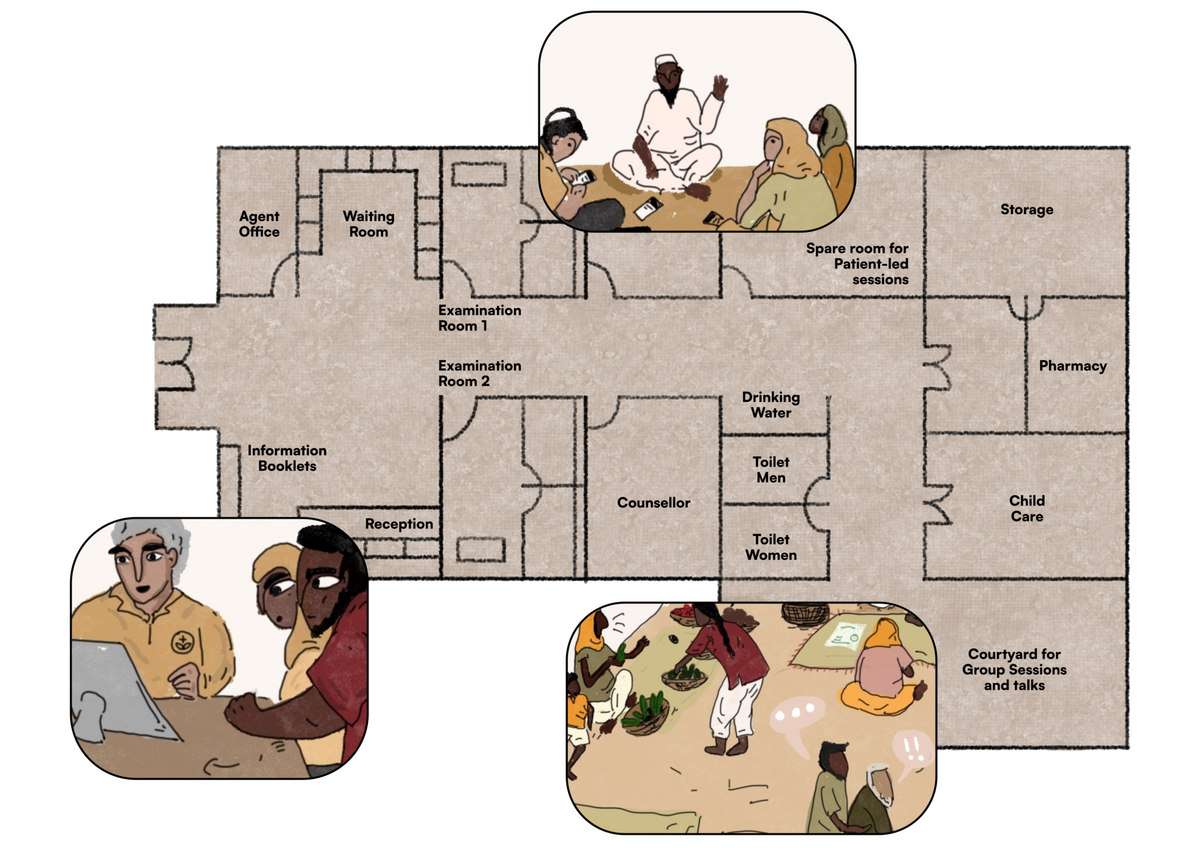
The Wellness Center builds on the idea of community clinics to provide not only direct healthcare but also other services, such as nutritional care, digital health services, health financing and support, that are direct healthcare adjacent, yet incredibly important to the overall health and wellness of an individual and the community in general. The Wellness Center reflects an understanding of healthcare as a journey that moves through diagnosis, recovery, continued care and recovery.
At present, health seekers, especially poor ones in LMICs, seek general wellness outside of the public health system. While the massive wellness economy serves the needs of those who are able to afford it, others have to rely on their social care networks and at times, alternate care practitioners. Within public health systems efforts to provide more comprehensive care and realize the potential of networks of care remain within some specific public health interventions, such as HIV/AIDS care. These efforts have largely been successful in improving health outcomes. Another example of a similar concept running through a PPP model is that of Philips Community Life Centers based out of Africa. These Centers provide vital primary care but also go beyond that, turning health facilities into community hubs where technology is bundled with additional service offerings, and can be created as new stand-alone facilities or be implemented in existing facilities.
In the future, public health systems could more formally recognise the holistic health and wellness needs of health seekers and bring these services closer to communities, and within the public health ambit, making access to wellness easier, especially for vulnerable populations. Building on present day efforts, this will entail considering health strands other than physical health. Additionally, it will involve recognizing networks of care, utilizing health volunteers, and providing points of contact for health seekers at various stages of their journey:
Implementing this concept would require heavy financial spending for the creation of new spaces. Alternatively, the focus could be shifted to bringing in and training the right resources in the existing spaces like community clinics, sub-centers, or primary health centers. In either case, there would be a high financial investment needed to reach the intended goal.
Remuneration and incentives for health volunteers and frontline workers, who are often women, are rarely adequate. Ideas like the wellness center require high levels of community participation. Sustainably incentivising this participation remains tricky and requires innovation.
Given a high dependency on human resources, it might be difficult to ensure the non-digital fringe healthcare services will be standardized across geographies. Program designers would need to pay close attention to training, monitoring, and regulating the health system touchpoints in these wellness centers.
Framing opportunities is an early step towards addressing these challenges.
-
How might we standardize quality control measures such that the healthcare workers or volunteers feel supported and incentivised to take up the desired role, without overburdening them?
-
How might we integrate new programs and resources in the existing system in order to reduce the financial strain on the system?
-
How might we create back-end channels for the healthcare workers or volunteers to receive consistent support or information when required so that they can confidently provide the services to the health seekers?
-
How might we work with the local influencers and leaders in the community to expand healthcare to actively include verified wellness related care and increase demand for these services?
-
How might we design innovative incentives for community participation including health volunteers?