Strand Based Seeker Profiles
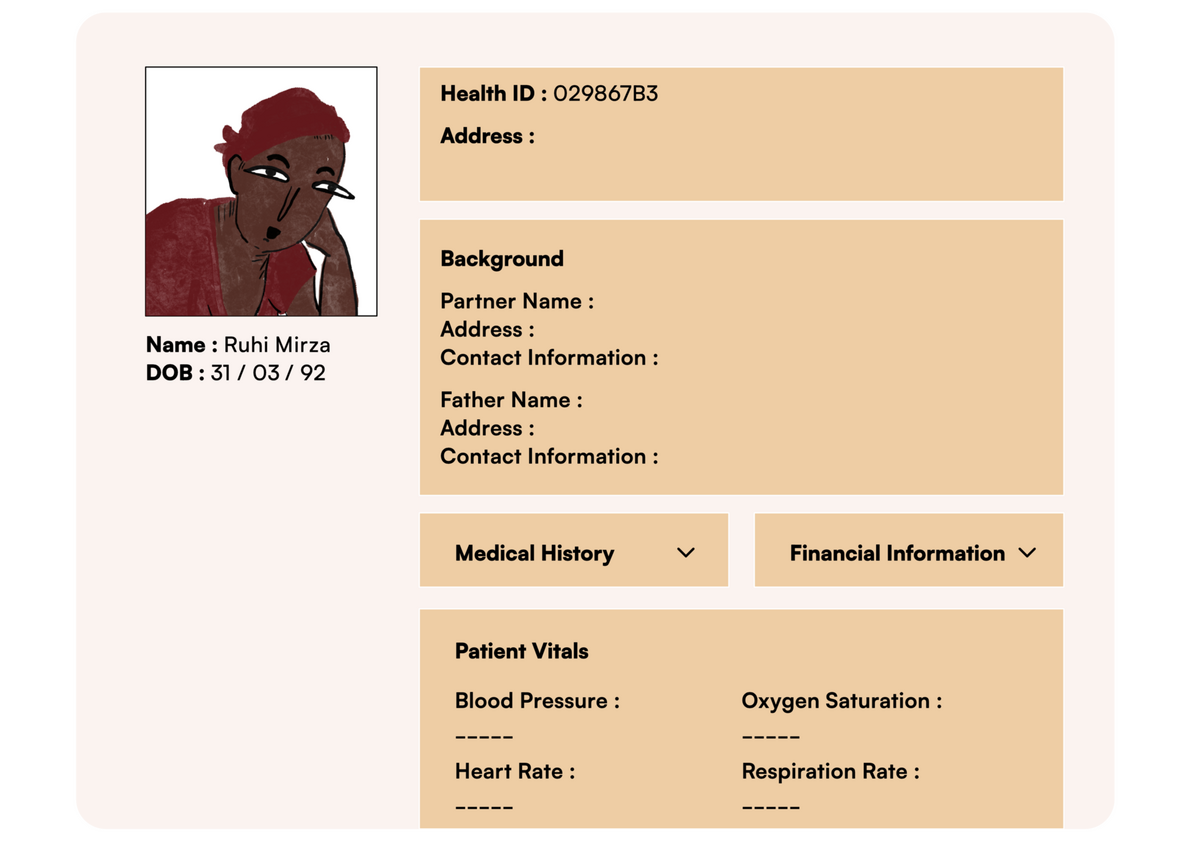
The health seeker profile is a combination of a medical record as well as a description and evaluation of other critical factors that could influence their health-seeking behavior. These factors include their financial status (financial health), their living conditions (environmental health), their mental/emotional health, and the strength of their social network (social health) that can support them during medical crises.
At present, task orientation, reinforced by practices within a biomedical model of care, can result in care that does not recognize the unique needs of seekers and is impersonal even if it is effective in improving aspects of clinical care. Research shows that when care is focused on procedures such as weight monitoring, blood tests, or drug prescriptions, the wider health and social needs of clients may be neglected. Surveys have shown that hidden social challenges can lead to misdiagnosis and a path of inappropriate investigations and care plans; some such social challenges cited include failing to ask about exposure to violence in the work-up of pelvic pain, prescribing medicines that patients cannot afford, lack of transportation to clinic visits, not understanding poverty and seekers’ inability to feed themselves, among others.
In the future, an expansive view of an individual’s health can be aligned with what they often see as constituent parts of their health. A more resilient health system can be designed in a more seeker-centered manner by accounting for these constituent parts– to cater to communities’ needs by understanding the vulnerabilities and strengths of individual health seekers. Further, addressing the social determinants will be seen as an important and emerging area of practice that entails starting earlier and broadening the scope of interventions, thus making entire families and communities healthier.
However, enabling the creation and use of such profiles will require addressing a few challenges:
Some of the relevant information might be considered personal by people and may limit them to openly and comfortably share these with health providers. ARC research shows that disclosing personal information like weak dietary habits, poor living conditions, poor mental health, or unfiltered drinking water causes shame and fear of judgement and is rarely shared by people. Further, when seekers do not trust the system to have their best interests in mind, it becomes harder to create an atmosphere where they can share this openly.
The implementation of the concept has a heavy reliance on the health workers who would be filling out these details and having these discussions. Since some of these details might be personal for the health seekers, it would be the health workers' responsibility to be empathetic and understanding with the seekers. The concept would also rely on new positions being created in the health system or rejigging of supply-side setups to ensure that the providers have enough time with the seekers.
Since this requires collecting and storing personal information, the health system would need to design systems for identification, storage, and upkeep. It would further require the providers to explain the process of data collection and storage to the seekers in order to obtain their consent to collect this information for medical purposes.
Framing opportunities is an early step towards addressing these challenges.
-
How might we support healthcare providers and staff members to create more safe spaces for health seekers to share relevant details about their different health strands?
-
How might we design processes, tools, and training, like standard questionnaires for health providers so seekers are comfortable with sharing and providers have the sufficient know-how and ability to engage with sensitive personal information?
-
How might we create easy-to-build seeker profiles such that healthcare workers are able to fill them easily/gain access to appropriate information from other legitimate sources?