Seeker-centric Support Structures
Seeker-centric support structures provide customized support to active and potential health seekers and communities before, during, and after the disease diagnosis. These support tools include:
-
Physical booklets to support illness management: This is a non-digital intervention to include health seekers who are usually not tech-enabled. For example, for elder seekers not comfortable with technology, the booklet is a way to engage and involve them in their care journey, and keep track of their healthcare information including test results, prescriptions, progress reports, contact numbers, and FAQs.
-
Digital resources for easy access and self-management: Such resources can be used at scale using digital mediums designed appropriately for less literate populations. These can be SMS-based reminders, voice-recorded messages, online and offline reminders and applications, among others.
-
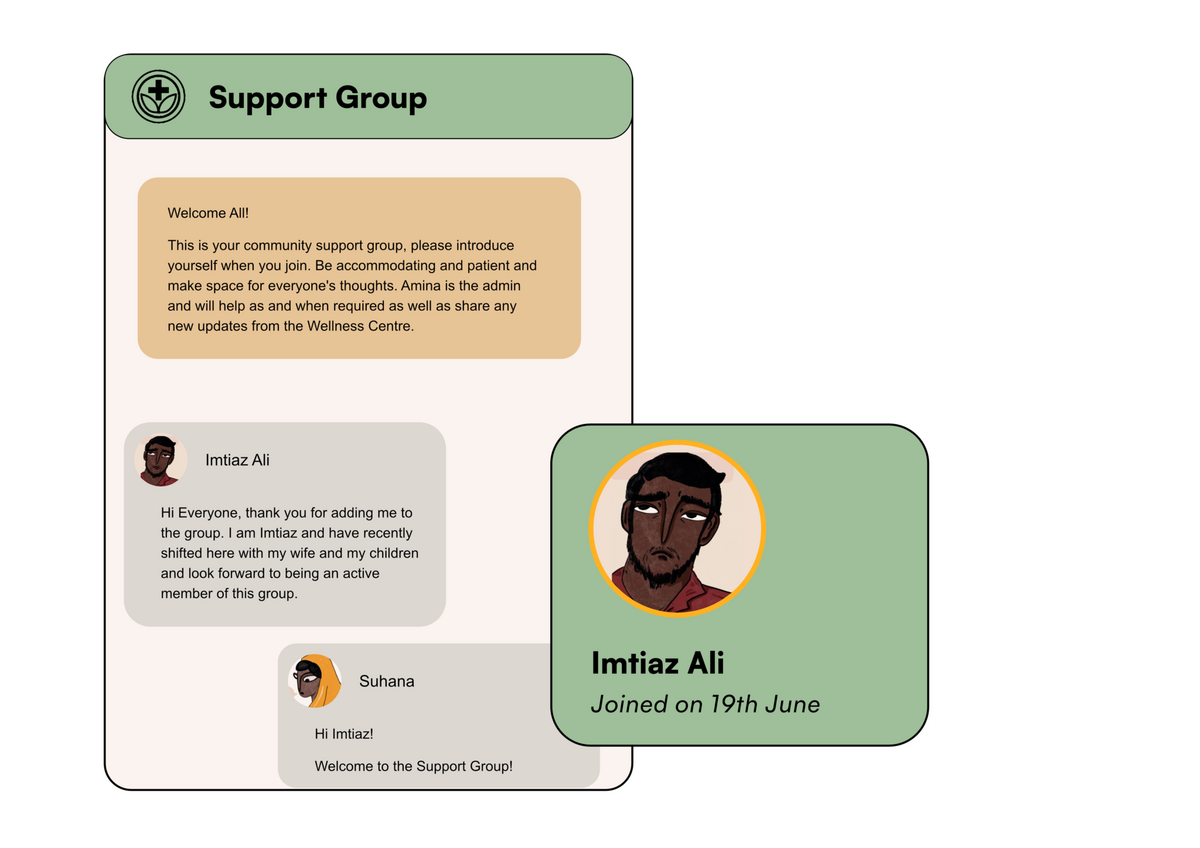
Facilitator-led shared spaces for health seekers: Such spaces aim to help seekers manage all the strands of their health by way of active support and sharing in smaller groups. These spaces are moderated by health actors or volunteers in-person, on a chat platform like WhatsApp, or in a hybrid setup.
Today, poor health seekers have limited resources to actively manage their illnesses. More often than not, they rely on their health providers to access information regarding disease management or preventive measures post-illness. While some interventions have been tried out to address this, a lot of them are designed as pathways for the system to reach out to the seeker, and not the other way round. This limits the seekers and their network’s ability to actively and timely participate in their care journey.
For example, there are interventions related to managing pregnancy like Mom Connect in South Africa that provides access to vital information to the mothers for managing a healthy pregnancy and safe labor. Studies show that clear, unbiased, and proper information improves patients’ understanding of their treatment, increases awareness of benefits and risks of medication, and sets realistic expectations, which improves adherence.
In the future, chronic disease burden and antimicrobial resistance (AMR) are predicted to surge, impacting low-income countries disproportionately. These create a massive financial burden on respective countries and invariably increase the pressure on the healthcare system as well as the affected families. Research has shown that one of the biggest reasons for the rising chronic disease burden and AMR is the lack of knowledge and awareness of the disease and its adherence practices among other behavioral risk factors. The growing acknowledgment regarding these in the global health communities holds the promise of more pointed action and investment to address these issues. In the future, addressing both NDCs and AMR will require working with communities on behavioral risk factors, increasing knowledge and awareness of the diseases, and equipping them (and their networks) with tools to play a more active role in their health journey.
However, there might be certain challenges that the program designers would need to address before scaling. These are as follows:
The program design may run the risk of dwindling impact if intervention sustainability and financial viability are not thought out. Successful mass customization of care in healthcare may require high financial investments and innovative models for ensuring sustainability.
While better prepared seekers who are willing and able to take a more active role in their healthcare journey will likely improve health outcomes, this is a need to ensure that the burden of care does not shift to the health seekers. With many seekers unable or unwilling to partner in their care journey, it is crucial to ensure that they don’t fall through the cracks.
Framing opportunities is an early step towards addressing these challenges.
-
How might we explore partnerships with private sector stakeholders to build seeker centric support structure and tools?
-
How might we intentionally design more wellness-related solutions and resources for easy uptake by seekers who have poor financial health?
-
How might we include more public engagement and communication experts to create intentional resources for positive behavior change at the end mile?
-
How might we engage and regulate informal care providers (who provide certified treatments like homeopathy, ayurveda) to build a salience for the broader idea of seeker-centric care support and create a channel for them to amplify the resources further?
-
How might we communicate the importance of the seeker support resources such that there is greater demand and incentive to create these sustainably at scale?